Innovation Reflections: Beyond the Robots and Flashy Gadgets
Last week I had the privilege to dive into the transformative world of healthcare innovation in Nova Scotia. It was inspiring to reconfirm that innovation isn't merely about surgical robots or high-tech advancements (which are super cool!). True healthcare innovation lies in reimagining processes, making the lives of our care providers easier, and focusing on the well-being of patients, their families, and the larger community. Here’s what I am taking back to New Brunswick after my time in Halifax.
Innovation Beyond the Flash: Innovation isn't solely about surgical robots or high-end tech. It's deeper – reshaping how we work and laying a solid foundation for the present and future so we are prepared for what comes next (like the robots).
Simplicity Can Be Revolutionary: Transitioning from paper to electronic scheduling for nurses can be transformative. It's about reducing administrative burdens and amplifying what our health professionals do best, caring for their patients.
Courage to Question: Keeping what works and having the bravery to challenge what doesn't, regardless of its size, is the essence of innovation.
Cultivating Change: We need a culture that encourages experimentation, accepts pivots, and celebrates the journey of innovation, not just the destination.
Breaking Barriers: Silos, bureaucracy, and rigidity have no place in a forward-thinking sector. BUT there are standards and values that must be protected and held at the front of this work. Our non-negotiables? Patient-centeredness, empathy, compassion, and humanity.
Informed Decisions: Using data not to generalize but to individualize care. One size doesn't fit all, especially in healthcare.
Holistic Patient Understanding: Recognizing a patient's full life experience to understand its impact on their health. Their story matters.
Leadership & Equity in Healthcare: Leadership in healthcare is about more than just titles; it's about nurturing inclusivity, championing flexibility, and sparking innovation. When women lead in the healthcare sector, they bring diverse perspectives, enhance patient-centric approaches, and foster environments that prioritize empathy and collaboration. Such leadership not only elevates the sector but also imparts positive, tangible impacts for patient health outcomes and the larger community. While we celebrate strides made in gender representation, we must remain committed to amplifying racial diversity and ensuring pay equity. As our communities grow increasingly diverse, our leadership should reflect and honor this beautiful diversity.
As I reflect on these insights, it becomes abundantly clear that true innovation is a harmonious blend of technology, process, culture, and leadership. It's about bridging the gaps, challenging norms, and advancing change that resonates deeply within our communities. The future of healthcare in New Brunswick and beyond holds boundless potential, and I'm filled with optimism. With continued focus on both the tangible and intangible facets of innovation, we are paving the way for a healthcare system that is resilient, inclusive, and truly transformative. As we stride forward, let's keep these principles at heart, ensuring we create a world where every individual feels seen, heard, and cared for.
Introducing my unconventional, creative & anything-but-linear job as a problem solver.
Hi there! Welcome to my little corner of the internet. I am a facilitator, a problem solver and the founder of She Consults. I guide and help organizations solve complex social problems. I approach problem solving using the design thinking process along with a side of curiosity, creativity and collaboration. I don’t do anything small; I believe the impossible is possible and I challenge my clients to think big too. The big problems deserve dedicated time and space under the microscope. My job is to create that space for clients to do the important work of solving the big problems of today. I craft and facilitate customized workshops and tools to empower clients as they work through the design thinking process. I am right by their side, acting as their problem-solving buddy.
“You are a facilitator and problem solver? What does that even mean?” I hear this so often, and four years ago I would have been asking myself the same question. What I do isn’t a traditional job, therefore people don’t always understand what it is I actually do, what a typical day looks like, what my work process is.
Hence, this blog post. Buckle in as I introduce you to my unconventional, creative and anything-but-linear process (because twisty turny paths are where all the learnings are, right?).
When a client first reaches out, they more often than not come to me with a vague idea of the problem they’re trying to solve. They are often concerned with the symptoms of the problem, and sometimes even unaware of what is causing the problem itself. A big piece of the process that I take teams through is digging deeper to uncover the root cause. Approaching the problem’s root cause ensures a higher level of success in implementing the solution and making sure it is adopted long term, in turn completely eliminating the symptoms the client initially came forward with and lowering the chances of the problem and its symptoms recurring. If we think of an iceberg, what we see above the surface is only a piece of the whole, but because we don’t see what’s underneath we don’t realize how big the iceberg actually is. We need to go below the surface—to truly understand the size of the issue—so that we can move forward with a full picture and understanding of all the angles and the magnitude of the problem.
Before I sit down to start designing workshops for a client, I need to familiarize myself with what the client is hoping to get at the end of the process, the proposed problem and any past key work that the team has done surrounding the problem in focus. I spend a lot of time prepping before the workshops even begin. I research the problem, watch videos, and read articles and studies. I listen to podcasts or talks from experts. I also try to understand what type of work has already been done by this team and others to solve the problem. I achieve this by talking with my clients and asking specific questions in addition to reading past project reports, funding applications and any other relevant documents. The final piece that I like to think about before designing a workshop for a client is, What is the goal of the workshop? What are they hoping to achieve? By deepening my understanding of the problem, historical work and desired goals for the workshop, I can then begin to design a path forward for my client.
Because more often than not, I am working with complex, systemic problems that have yet to be solved, there lives uncertainty: uncertainty about where to focus, uncertainty of roles and responsibilities of those around the table, uncertainty about which solutions to implement. The work is blanketed in uncertainty, and that is uncomfortable for us as humans, who crave the comfort of knowing, routine and linear, clear paths.
To combat the fears that arise from uncertainty, I try to support groups by aiding them in building a strong team foundation. I believe that anytime groups come together to tackle big problems, there should be work done on the front end to ensure the team is ready to move together, at the same pace, towards the same goal. But creating this alignment takes concentrated energy and time. Teams often skip this step, deeming it nonessential. But I argue that it is one of the most essential steps in shoring up the future success of a team, and ultimately their outputs, because team members can lean on each other when the fear of uncertainty creeps in, threatening to dismantle the work.
Thus, one of my first steps is to create and hold space for the essential team building work to happen. I have found over time that the secret to crafting the perfect environment conducive to problem solving and team building is to encourage creativity, collaboration and vulnerability.
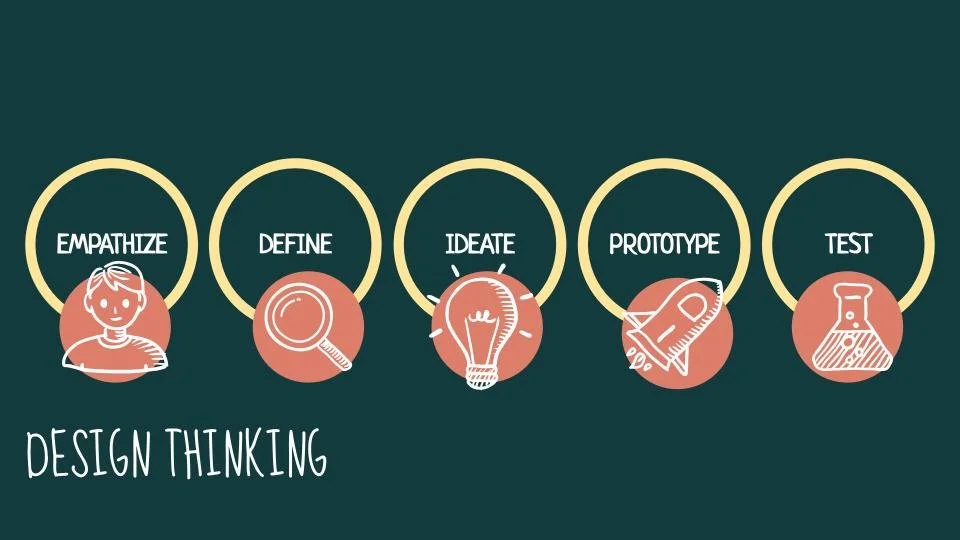
Once I sense that we are working from a solid foundation built on trust and centred on a mutual understanding and common goals, we’re able to dive in. At that point, I introduce a process called design thinking.
Design thinking is a process used to solve complex problems. A problem becomes complex when the path towards solving it seems convoluted and unclear. These problems have been unsolvable for a long time, centuries even, for a variety of reasons: ingrained and outdated mental models, systemic challenges, hurtful patterns and a lack of understanding of root causes.
Design thinking uses a human-centred approach that revolves around a deep interest in developing an understanding of the people who are the most impacted by the problem and with whom we’re designing the products or services.
Empathize: truly understand your user so that you can co-create meaningful solutions that support their needs, remove any barriers and/or challenges they face, amplify their hopes and minimize their fears.
Define: based on what you have gathered and learned about the user, apply a curiosity mindset and clearly define how you (and your team) might help the user solve a problem. The Empathize phase was all about understanding the user, while the Define phase is all about understanding the problem and how it impacts the user’s life.
Ideate: Now that the problem is clearly defined, which has provided direction, it’s time to explore possible solutions. This phase requires teams to refrain from judgement. No idea is off the table: even what might seem like a wildly outrageous idea may end up being a refined version of the final solution. We don’t want to limit our possibilities yet, and judgement does just that. By starting big and then narrowing, we ensure all ideas are explored and evaluated and the best possible solutions are picked to tackle the problem.
Prototype: Get your craft on. Pull out the construction paper, the glue sticks, the glitter and Lego: it’s time to build prototypes of your solutions. You don’t need to spend a lot of money or time to gather valuable feedback about your proposed solutions. Getting feedback early on in the process can make or break a project. If we open ourselves up to early feedback on a conceptual solution from the actual person whom the solution is designed for, then we can ensure that our solution’s intention aligns with the real needs of our user before we actually implement and spend tons of resources on a solution that doesn’t work. Prototypes allow us to test our ideas quickly, at small scale and low cost.
Test: Once the prototypes are built, it's time to gather feedback from the users. Does this help? Does this do what we intended? Is this sustainable? Take the feedback, integrate it into the next version of the solution, then gather more feedback. It’s a loop. This loop may seem tedious, but in the end, when you are ready to put real resources behind it, you can be confident it will be successful because you’ll have a fully fleshed out, user-tested and approved proof of concept.
The design thinking process is a guide to help a team move from problem identification to proven solutions. Within each phase of the process, there are tools and activities that are used to advance the team forward through the process. It is my job to select the appropriate tools, introduce and teach the tools, support teams as they use the tools and finally, capture and record whatever outputs and learning emerge from the tools. As a team moves through the design thinking process, I am taking the emerging data and learnings, recording it and presenting it back to the team constantly to ensure the next step is a progression of the learnings from the previous step. This record tells the story of the team and how they arrived at their proposed solutions. It also acts as a business case for those proposed solutions, to be used for work planning, funding applications, organizational restructuring, etc.
My expertise and official role ends once the team has gone through the entire design thinking process. I send the final report to my clients knowing that now that they have a set direction, they have the expertise and passion to go on towards implementing thoughtful solutions to big complex problems. I often stay linked to the project work even after I send that final email, because I become so invested in the team and the success of their solutions. My role shifts from process facilitator to cheerleader—cheering them on from the sidelines and offering additional support when and where I can.
My work days are never typical, because every problem is different, every team is different and these differences deserve and demand customized approaches and support. I thrive on this; the constant change challenges me to try things and to keep growing.
I am often confronted with concerns about timelines; there is an attached belief that to be innovative or tackle big problems in this way is time consuming and there isn’t time to spare because there are real people struggling right now. I have never been good at comforting those concerns, because they are right: there are often real, urgent needs that require immediate attention and action.
Let me try to comfort those fears here and now. I can confidently say that dedicated time and space allows for true, proactive problem solving that addresses root causes instead of just symptoms. But also, this proactive work can be done in parallel with meeting real and urgent needs. It doesn’t need to be either/or. We can fulfill current needs, like welcoming people needing a place to sleep into a shelter for the night, while also working towards creating a future where those needs don’t even exist and every person has access to their own warm and safe bed every single night forever.
This is my hope. The dreamer in me dreams of a world where communities and individuals are not only surviving, but thriving and flourishing. And the optimist in me believes I can play a small role in making that dream come true using design thinking.
My Postpartum Journey
We need to do a better job at taking care of our new mommas’ mental health.
It’s late November, 2020, and I’ve just recently had a beautiful, happy and healthy baby boy. I am eight days postpartum and baby and I are thriving physically. He is my second baby making our family a unit of four including his dad Dillon and his four-year-old big sister Sloan. We are overjoyed to welcome baby Gordon into our home and our hearts. He is only eight days old but I can already see that he is a sweet soul who loves nothing more than to snuggle and sleep. Lucky me! With a four-year-old running around and a shift-working health care employee for a husband, I am feeling beyond blessed to have such an easygoing and peaceful baby as we continue to navigate the transition from a family of three to a family of four.
I am blessed to have the support of a caring community of ladies and family members who have been nothing short of amazing as they help care for our little family by making freshly cooked meals, washing endless loads of laundry, inviting big sister Sloan on playdates and holding baby Gord so that Mommy can take a shower. I reflect on the past eight days and I recognize that I am extremely lucky. I am in awe of how this community has come together to care and love us during this special but chaotic time. I’m humbled and speechless—I’m not even sure how to begin to thank the many people who have opened their hearts to support us. I hope these words can act as a start in expressing my immense gratitude.
Over the past few years, I have learned a lesson that is reflective of my current situation in this life: things can be sweet and salty at the same time. While the past eight days have been filled with sweetness, love, and community, it has also been salty and extremely difficult.
I’ve had my struggles in the past with anxiety and depression. Like many, I struggled as a teenager and a young adult, trying to figure out who I was while balancing poor mental health. I dealt with severe anxiety when I had my first child four years ago and I had another slip into darkness about two years ago. All of these times, I was able to persevere, get better and come out on the other side.
I am not someone who is shy to ask for help. After living with mental health struggles on and off for most of my life, I am educated and know what works for me and what doesn't. When I feel like I’m slipping, I immediately dig in and come up with a game plan to get myself feeling mentally well. These plans consist of techniques and supports I’ve learned over the years:
cut out anxiety-inducing foods like caffeine and sugar,
seek counselling support,
reach out to my doctors to evaluate my medications,
meditate,
write in my gratitude journal,
talk it out with friends,
introduce exercise,
and force myself to do little things every day like take a shower or make my bed.
I have become an expert at getting myself better. I am tenacious, and I don’t accept that bad feelings will be my normal. But even though I am this expert, it never gets easier when I find myself falling. Yet the opposite; it is still the most terrifying experience. It is absolutely brutal. It’s like I can’t breathe. Even though I know it will pass, that I will come out the other side, hopelessness settles into the pit of my stomach. Every time.
I was optimistic that I wouldn’t have any mental health struggles after my baby boy was born. I have been symptom-free for almost two years, the pregnancy was a breeze, and I felt that since this was my second baby, I would be more in control. I was wrong.
I am little more than a week postpartum and unwelcomed companions have paid me a visit: anxiety and depression. It is debilitating. I can’t eat, I am unable to feel joy, and feelings of vast sadness have overtaken me. But I know what to do. I know I can get better and I desperately want to so that I can enjoy what is supposed to be a happy time at home with my family.
First step is to ask for help. I reach out to my OB/GYN (who had previously stated that he would help if any old mental health issues arose postpartum) via phone and email. I then reach out to my nurse practitioner and leave her a message to call me as soon as possible. I immediately stop drinking coffee, vow to shower every day, and force myself to eat my three meals a day even though I have no appetite and the thought of food makes me sick. I continue to take care of my newborn, waking up with him every three hours to breastfeed, change diapers, snuggle him and love him. I am lucky to have my husband and mother-in-law home with me, who take care of household chores and meal prep. On top of all of this, we are driving two hours every other day for baby’s doctor appointments.
I feel I have done all I can do; I’ve reached out for help. I am in indescribable emotional pain as I wait for a response from my OB/GYN and/or nurse practitioner. It is an emergency—I know I need help fast. But I keep telling myself that I just have to hold on; it will get better. I wait for days in pain with no helpful responses when what I need is immediate action from my health care team.
I call the doctor’s office multiple times with no answer, so I leave a message. Radio silence. So I send an email explaining my situation and plead to speak with someone. I hear back via email! I am so relieved: finally, someone. I am informed that the doctor isn’t in the office but that they’ll try to contact him for me. I am also instructed to reach out to my nurse practitioner (which I already have).
Again I am left waiting for someone to get back to me. All the while I am trying to be strong and keep it together at home. Limiting caffeine, eating my meals, changing diapers, feeding baby, entertaining my four-year-old, repeat. On the outside I probably look like a zombie or a robot. On the inside I am a heaping, crippled mess of fear, self-hatred, and pain.
I receive another email from my OB/GYN’s office. My doctor is going to attempt to call me in the evening, after his work day. I feel I can finally breathe a little easier. I just have to wait an hour or two and I can talk to someone who’ll assist me and my recovery efforts. I wait an hour, then another, then another. I tell myself maybe he’s running late, just be patient, he will call, he knows how urgent this is. He never calls. I am devastated. I go to bed feeling the deep, deep all-consuming emotional heaviness, with no end in sight.
The next morning I follow up with an email. Will the doctor be calling me today? I am told that he is in the operating room all day but that he will contact me as soon as he can. Again, I am instructed to reach out to my nurse practitioner as well. At this point it makes me feel like they are trying to pass me off as someone else’s problem.
I can’t wait any longer for my nurse practitioner or OB/GYN. My mental health state is not improving, and each minute that goes by feeling this way is too much. I google after hours clinics. I find one located forty minutes away. I call and I am able to get an appointment the next day. YES!
After acquiring my appointment at the after hours clinic, I receive a phone call from my OB/GYN’s assistant which leaves me feeling worthless and dejected. I am informed that the doctor won’t be calling me, that he doesn’t usually deal with these types of matters, that his job ends once he’s delivered his patients’ babies. The lady on the phone again encourages me to reach out to my nurse practitioner (who still hasn’t called me back). I let her know that I called a local clinic and I have an appointment the next day. She seems thrilled for me. She asks me to document everything I have done up to this point and the outcome of tomorrow’s appointment in an email so that the doctor can “be kept in the loop.” I feel deflated. I feel hurt. I feel betrayed. My main focus is to get better and I realize then that he isn’t going to help me with that. (I never did write that documentation email. Maybe I should have. But I couldn’t be bothered to help that doctor cover his ass.)
I talk to the doctor at the after hours clinic, he listens, and together we come up with a recovery strategy. He increases my medications slightly and introduces medication to take as needed if things get too bad. We talk about my counselling options and he asks me to follow up with him in three weeks.
Finally, I’ve gotten what I need from the medical community: a doctor who responded to my urgent healthcare need in a timely manner, who listened and recognised my pain, who included me in creating my recovery plan and who promised to follow up. Hallelujah.
Throughout my pregnancy, up until we left the hospital with our baby boy and before my anxiety and depression started, I was told that the baby blues were normal. That's what I kept hearing over and over again. It’s normal to feel sad. Then the emotional turmoil started, and those words did nothing to comfort me. The postpartum depression/postpartum anxiety literature sent home with me in my hospital bag, the countless experts in the maternity ward reminding me of the potential threat of the baby blues, then the reassurance and reiteration that my feelings were normal at the mommy and baby clinic, they were just empty words. Empty words wouldn’t help me recover, wouldn’t allow me to feel joy again, wouldn’t drag me out of this hell. But words were all I got for a long time.
There wasn’t easily available help. I had to reach out to multiple healthcare professionals until I found someone who was interested in helping me. If I had a broken arm, a cast would be put on immediately. Why are mental health issues treated so differently? I was failed. But I realize it could have been much, much worse. What if I was too shy to ask for help? What if this was the first time I had ever felt this way and I didn’t know who to reach out to? What if I let the bad feelings take over and I gave up? It should not have been this hard to get help.
I am now able to provide an update on my mental health state. I have been on my new dosages of medications long enough to see improvements and I have connected with my new counsellor. I have seen my NP (she never did actually call me back) at my son’s post-birth checks and she is up-to-date and following my journey. How am I feeling? Every day is a struggle but it is so much better than it was in those early days. The bad feelings are duller, allowing me to focus on the other things that will help me to heal: fresh air, counselling, proper sleep, healthy foods and my caring community. I have reached out to my closest family and friends to share with them my struggles and they have wrapped me in love. I am on my way to recovery. The recovery road was dark and lonely for so long, but I can now see the light at the end of the tunnel.
I believe we can improve the health care system to support new mothers and their mental health. I don’t have all the answers, but I am interested in finding those answers. I believe a logical place to start is by making it easier to access mental health services for new moms. I hope that by sharing my story, it can start a conversation. In my work, we like to use curiosity to flip problems into opportunities for solutions. So here I will do that:
How Might We Support New Mothers and their Mental Health?
I will be continuing to explore this problem and possible solutions on my maternity leave. Anyone who would like to discuss or has interest in this topic please reach out! The biggest lesson I've taken from this whole experience is that a caring community is a powerful thing.